58
CLINICAL PRACTICE GUIDELINES
OUTPATIENT MANAGEMENT OF CONGESTIVE HEART FAILURE IN ADULTS
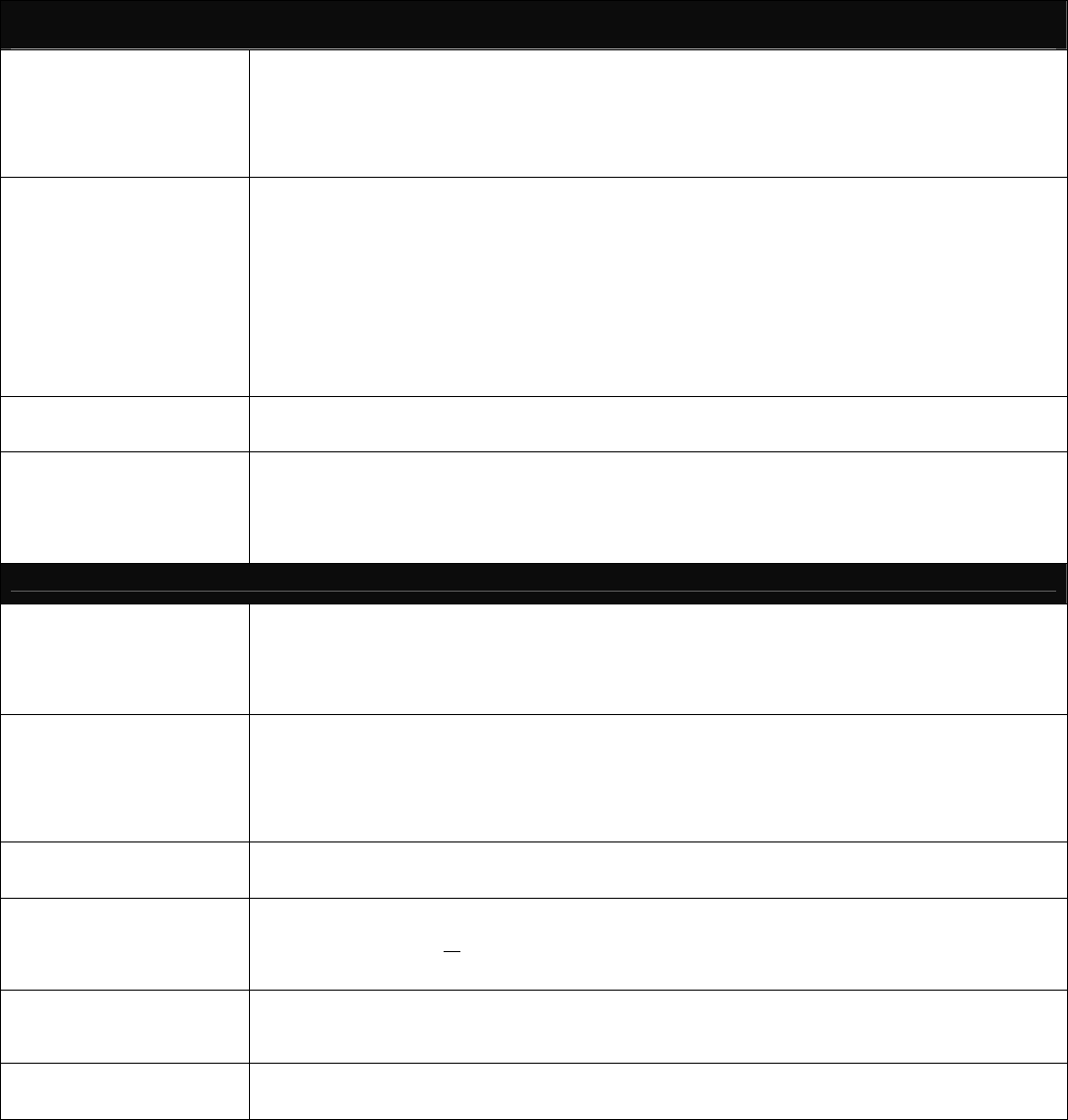
G
OALS FOR DIAGNOSTIC
EVALUATION
Establish Ejection Fraction and document the Left without resulting Ventricular Dysfunction
Determine underlying cause of heart failure
Identify precipitating or aggravating correctable factors
Develop Management and Treatment Plan
Provide baseline information to monitor effects of treatment
Establish baseline NYHA classification
INITIAL EVALUATION OF
HEART FAILURE
DIAGNOSTIC TESTING
Complete History and Physical Examination
Clinical Testing
Chest X-Ray, 12-lead Electrocardiogram
Assessment of Ventricular Function
Transthoracic Doppler 2-D Echocardiography
Radionuclide ventriculography
Evaluation testing for ischemia (Stress, Nuclear Test
OR Stress Echocardiography OR Cardiac
Catheterization) Complete Blood Count, Urinalysis
Fasting Lipid Panel, (Cholesterol Triglyceride, HDL Cholesterol, LDL and LDL: HDL Ratio)
Blood Chemistry: Electrolytes, BUN, creatinine,
Glucose, Liver function test and TSH level
ADDITIONAL DIAGNOSTIC
TESTING
Consider additional diagnostic testing for evaluation of other cardiac or non-cardiac related causes in the absence of ischemia
or Valvular Heart Disease, Serum Iron and Ferritin, Endomyocardial Biopsy, Phosphorus, Magnesium, Calcium and
Albumin levels
SPECIALTY REFERRALS
Cardiac Educator – As indicated
Nutritional Counseling – As indicated
Cardiology Consult – Consider consultation during the initial evaluation and anytime during the ongoing management
of CHF as appropriate
Home Health Care – Consider home health care for outpatient monitoring
Cardiac Rehabilitation Programs – Consider rehabilitation programs to maximize functional capacity
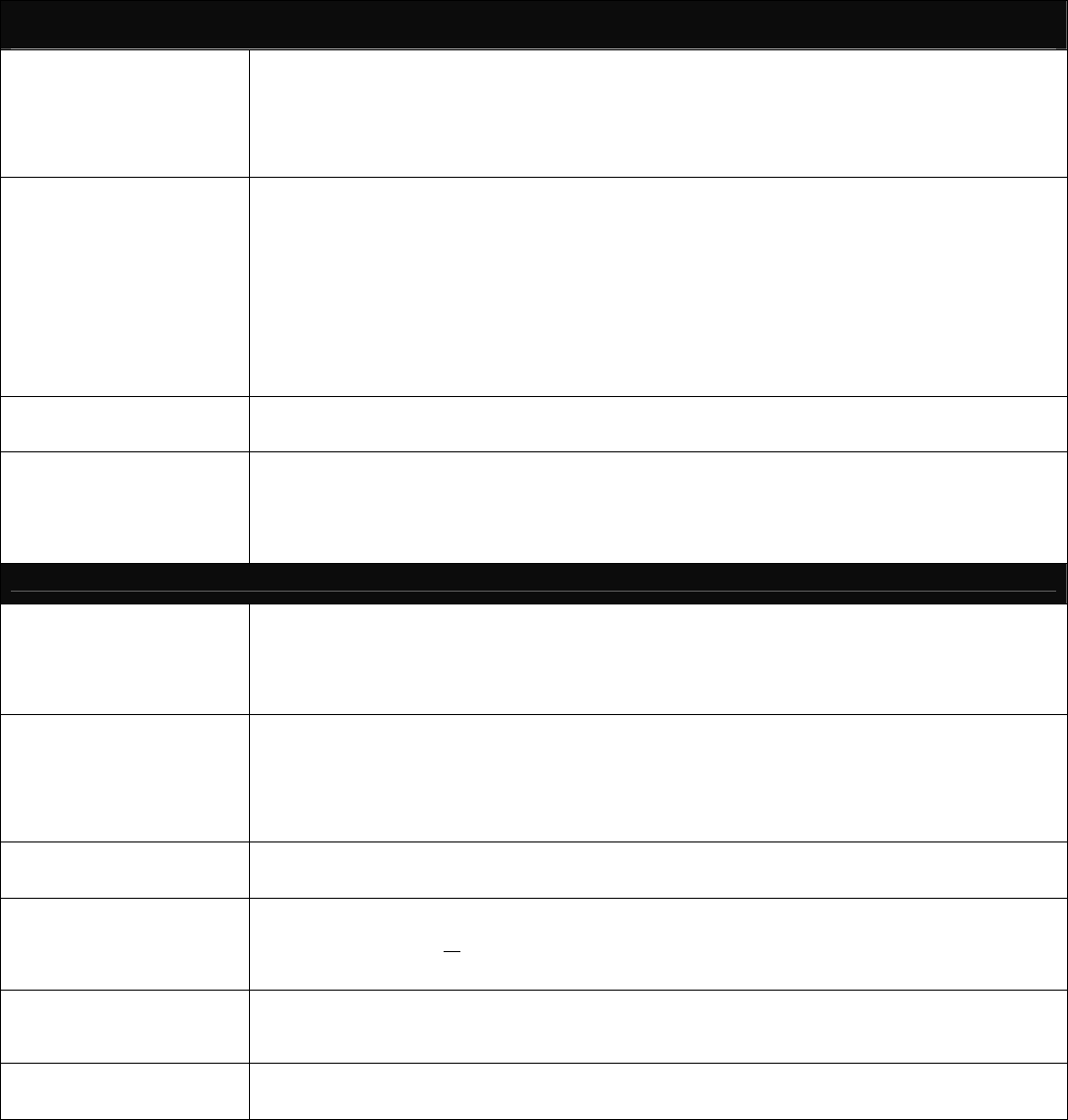
MANAGEMENT PLAN, EDUCATION & FAMILY COUNSELING
PATIENT AND FAMILY
EDUCATION AND
COUNSELING
Nature of heart disease-Drug Adherence Regimens
Symptoms of worsening CHF-What to do if symptoms occur
Mechanisms for complicated medical regimens-Coping
Presentation measures for further progression of the disease
Accurate information concerning prognosis should be discussed in order for patients to make decisions and plans for the
future. Discuss the planning of advance directives with patients and family in the context of heart failure management
LIFESTYLE
CHANGES/HABITS
Physical Activity – Recreation, leisure and work activity as tolerated
Exercise – Establish a regular exercise program consistent with individual patient’s capabilities and clinical status.
Program should be dynamic (walking, cycling) not isometric to pervert or reserve physical including drug doses.
Sexual Activity – Discuss sexual difficulties and coping mechanisms if they occur
Smoking Cessation – Emphasis on the importance of not smoking: medications of financial assistance determine the
willingness to stop smoking and strategies for smoking cessation should be tailored to each individual
Alcohol Usage – Discourage alcohol use
DIETARY MEASURES
Sodium restriction –Define and quantify the amount of salt that is allowed in the daily diet, 3 grams or less. (Personal
food preferences, culture, income and family support should be considered)
Management of Cachexia/Management of Obesity
FLUID MANAGEMENT
Establish baseline weight
Encourage daily weights on the same scale at the same time each day
Report weight gains of >
of 5+ lbs. in a week
Establish/monitor daily fluid intake limits; avoid excessive fluid intake
Instruct on fluid restriction if indicated
MEDICATION EDUCATION
Develop a patient medication schedule including drug doses
Review effects of medications on quality of life and survival
Discuss probability of side effects and what to do if they occur
Discuss availability of lower cost medications or financial assistance
IMMUNIZATIONS
Influenza (flu) –vaccine annually
Pneumococcal vaccine –initially/repeat as per CDC recommendations
**Utilization Management Committee will review Guidelines for new scientific evidence or national
standard changes prior to distribution to Providers annually.